
When it comes to opioid addiction treatment, the terms medication-assisted treatment (MAT) and medications for opioid use disorder (MOUD) are often used interchangeably. However, while both involve the use of FDA-approved medications, they carry different meanings in addiction treatment.
Understanding the difference between MAT and MOUD helps provide clarity around treatment approaches, promotes the use of evidence-based care, reduces stigma and supports those seeking recovery.
What is MAT?
Medication-assisted treatment (MAT) is an evidence-based approach that combines FDA-approved medications with counseling and behavioral therapies to support individuals with substance use disorders, including opioid use disorder (OUD) and alcohol use disorder (AUD). The goal of MAT is to help patients manage withdrawal symptoms, reduce cravings and prevent relapse while addressing the psychological and behavioral aspects of addiction.
MAT is a comprehensive treatment model that recognizes addiction as a chronic disease requiring both medical and therapeutic interventions. It includes:
- Medications to normalize brain chemistry and reduce withdrawal symptoms.
- Counseling and behavioral therapies to address underlying psychological and emotional factors.
- Wraparound support services such as case management and peer recovery support to promote long-term recovery.
MAT has been highly researched and is shown to improve treatment retention, reduce illicit opioid use, decrease the transmission of infectious diseases and lower the risk of overdose.

What is MOUD?
Medications for opioid use disorder (MOUD) is a more precise term that specifically refers to the use of FDA-approved medications to treat opioid addiction. Unlike MAT, which is a broader treatment framework, MOUD focuses solely on medication as a critical component of evidence-based care for OUD.
Why the Shift from MAT to MOUD?
Organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) and the National Institute on Drug Abuse (NIDA) have increasingly adopted the term MOUD instead of MAT. This change is meant to address a common misconception - “medication-assisted treatment” can suggest that medication is merely a supplement or temporary role rather than a primary treatment method. It was also believed that medication-assisted treatment substitutes one addiction for another.
In reality, MOUD is an essential, first-line treatment for OUD. By using MOUD, healthcare providers emphasize that medication is not just an “assistive” tool but a core component of effective opioid addiction care.
FDA-Approved Medications for MOUD
MOUD includes three FDA-approved medications – methadone, buprenorphine and naltrexone, which are the most common medications used to treat OUD. These medications work by reducing withdrawal symptoms, curbing cravings and stabilizing brain chemistry, allowing individuals to focus on their recovery. Since each medication works differently, understanding how each one functions can help individuals and providers make informed decisions about treatment.
Methadone
Methadone is a full opioid agonist that binds to opioid receptors (mu-opioid) in the brain to ease cravings and painful withdrawal symptoms. Unlike illicit opioids, methadone is taken in controlled doses under medical supervision, allowing individuals to stabilize without producing the euphoric effect of other opioid drugs.

As a Schedule II controlled substance, methadone is highly regulated due to its potential for misuse and dependence. It is only available through licensed Opioid Treatment Programs (OTPs), where patients typically receive their doses daily. Many individuals receiving methadone also become eligible for take-home doses, offering greater convenience and flexibility as part of their recovery journey.
Methadone is available in several forms, including:
- Liquid: The most common form dispensed at OTPs. It is often mixed with agents that make it less likely to be used in ways other than intended.
- Tablet: Can be taken whole or dissolved in liquid before being taken.
- Powder: Mixed into a solution before being administered.
Methadone has been used for decades and is one of the safest and most effective treatment options when taken as prescribed. Because it’s a full agonist, it is important that patients follow their prescribed treatment plan, as improper use can increase the risk of misuse and overdose.
Buprenorphine
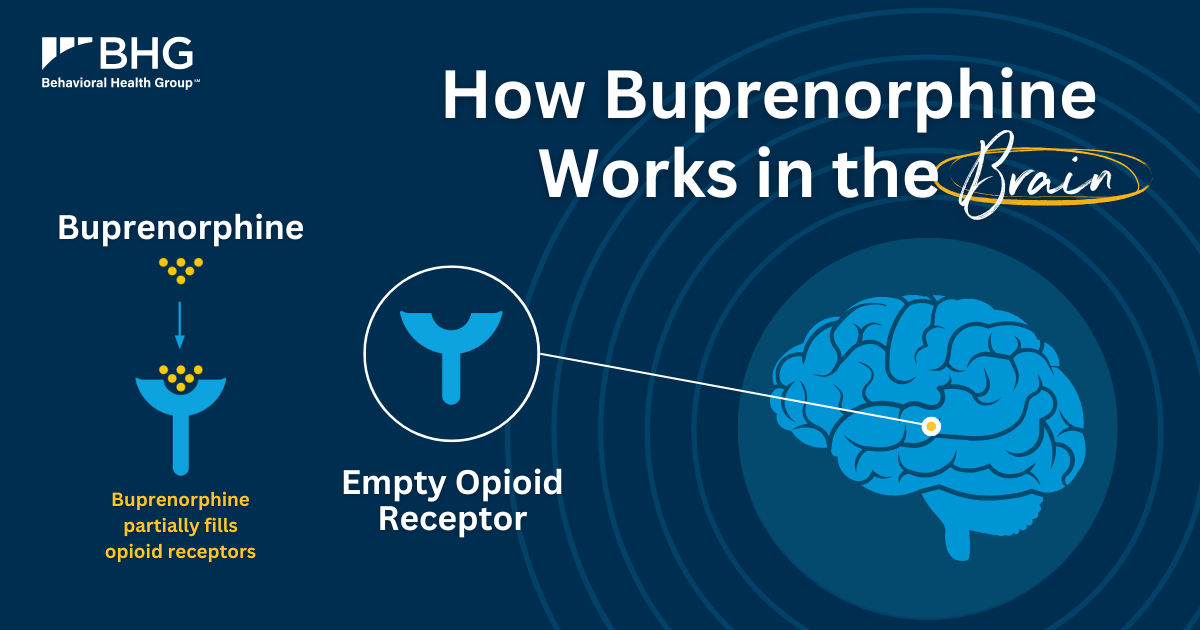
Buprenorphine is a partial agonist, meaning activates opioid receptors to a lesser degree. Like methadone, it effectively provides relief from painful withdrawal symptoms and cravings while lowering the risk of misuse and overdose. It also does not produce euphoric effects and does not have dangerous side effects associated with other opioids.
As a Schedule III controlled substance, buprenorphine has a lower risk of misuse compared to full opioids, though it still requires careful prescribing and monitoring. It is available in different forms, including:
- Buprenorphine/naloxone: Available as a film or tablet.
- Buprenorphine-only tablets: Often used in certain cases, such as during pregnancy or when someone has a sensitivity to naloxone.
- Extended-release injection: Administered monthly for long-term treatment.
Unlike methadone, buprenorphine can be prescribed in both Opioid Treatment Programs (OTPs) and Office-Based Opioid Treatment (OBOT)/Office-Based Addiction Treatment (OBAT) settings, making it more accessible. Many patients benefit from the flexibility of at-home dosing, which allows them to continue their daily lives while receiving treatment.
Naltrexone
Naltrexone is an opioid antagonist, meaning it binds to the mu-opioid receptor without activating it, effectively blocking the effects of opioids if they are used. The medication also does not produce any euphoric effects, so no physical dependence is associated with their use, making it an effective tool for relapse prevention and for abstinence-based treatment, not for withdrawal management.

In addition to treating OUD, naltrexone is also FDA-approved for alcohol use disorder (AUD), helping reduce alcohol cravings and lower the urge to drink.
It is available in two forms:
- A daily oral tablet that must be taken as prescribed.
- Vivitrol: An extended-release injectable that is administered every four weeks, or once a month by a practitioner.
One important consideration is that individuals must be opioid-free for a period of time before starting naltrexone. Taking it too soon can lead to sudden and severe withdrawal symptoms, which can make the transition into treatment more challenging. Because of this, naltrexone is often recommended for patients who have already cleared opioids from their system and are looking for a non-opioid option to maintain long-term recovery.
MAT vs MOUD: Key Differences
While MAT and MOUD are closely related, they are not identical. MOUD refers to specific FDA-approved medications for opioid addiction, while MAT is a broader approach that combines these medications with counseling and behavioral therapies.
The table below outlines the key difference between these terms:
| Aspect | MAT | MOUD |
| Definition | An evidence-based, whole-person approach that combines medication with counseling and behavioral therapy. | The use of FDA-approved medications specifically for opioid addiction treatment. |
| Scope | Used for opioid use disorder (OUD) and alcohol use disorder (AUD). | Applies only to opioid use disorder (OUD). |
| Treatment Components | Medication + therapy + support services | Medication-focused. |
| Goal of Terminology | Describes the comprehensive treatment model. | Reinforces that medications alone are an evidence-based treatment for OUD. |
Why This Distinction Matters in Addiction Treatment
The difference between MAT and MOUD is more than just terminology – it shapes public perception and treatment policies. The term “medication-assisted treatment” can suggest that medication is only a supplement rather than a main treatment or it substitutes one addiction for another, reinforcing stigma and misconceptions. MOUD is the preferred term because it recognizes that FDA-approved medications are essential, evidence-based treatments for OUD. By shifting the language, we help validate these medications as standard medical care to help to reduce stigma and encourage more individuals to seek treatment.
Today, MOUD is widely used in clinical guidelines, research and treatment policies to ensure clarity and consistency. As more providers and policymakers adopt this terminology, it supports a more effective, science-driven approach to care. Recognizing the distinction between MAT and MOUD is key to improving and expanding access to care and improving public understanding of OUD.

Find Effective OUD Treatment at BHG
At Behavioral Health Group (BHG), we provide evidence-based OUD treatment that integrates MOUD with counseling and wraparound services. We are one of about 4% of providers nationally that offer all three FDA-approved medications – methadone, buprenorphine and naltrexone. By offering all available medications, our physicians and other clinical staff can tailor treatment plans to meet the unique needs of each patient and ensure they are set up for success.
If you or someone you know is seeking treatment for OUD, help is available. Find a BHG location near you and call 844-535-7291. Healthcare providers and referral partners can reach out through our referral line at 866-763-2244 or submit an online referral form.
© 2025 BHG Holdings, LLC. All rights reserved. Trademarks are the property of their respective owners.
